I recently wrote a post called “Dairy Me” in which I proclaimed my excitement to the world about how my family is officially no longer dairy free. I described the method we used to introduce dairy to Winston (and previously Carter), following the specific instructions of an allergist. In this post I also noted that we were not performing endoscopy and biopsy procedures to check for the presence of eosinophils, which would indicate that the dairy was causing a flareup of Eosinophilic Esophagitis. We made this decision based on the opinion of that same allergist, who assured us that if an allergen was in fact a trigger food, then Winston would begin to display symptoms and we would know for sure.
For the most part, the public response I received was very positive; everyone was congratulating us on our latest food allergy milestone. But when I shared my post on a pediatric EoE support group page, a few mothers chimed in with their opinions. One wrote (paraphrased):
“How do you know that you aren’t doing damage to his esophagus without scoping? My child has had no symptoms [for 3 years] but still fails his scopes.”
To which another mother replied:
“She doesn’t.”
Ahem.
I thought about responding with the words that immediately filled my head, but then I would have stooped down to this woman’s level. So instead I just removed my post and reassured myself that some people simply lack, oh what’s the word… ah yes, tact.
What I believe this woman meant to say to me was:
“It is my understanding that just because one doesn’t have symptoms from a food allergen, doesn’t mean that food allergen isn’t an EoE trigger. You can still be damaging the esophagus without presenting any symptoms. You might want check with your physician about this. Best of luck though! [heart emoji]”
You know, in a supportive way. Because after all, isn’t that what an EoE support group is for? To build up other moms who are dealing with their kids’ food allergies, not to belittle them on social media.
But all rudeness aside, these comments did get me thinking… and researching. Sure enough, the very first website I clicked on confirmed what was said. The Kids with Food Allergies Division of the Asthma and Allergy Foundation of America states that “sometimes, foods that people eat regularly may be triggers, even ones that were never associated with symptoms. This is the difficult part of EoE… Eosinophils can be triggered by a food with minimal – or in some cases – no symptoms… Symptoms are not a reliable way to monitor one’s EoE. Repeat biopsies are necessary to directly see how an individual responds to treatment.”
I felt like the floor was ripped out from underneath me. Here I am thinking we are moving forward, getting out of this horrible phase of our lives, and suddenly now we are taking a step back. What I thought was a sure thing – no symptoms, no allergy – was not. Then my mind flooded with questions.
Could Carter be showing no symptoms, but his eosinophils are back from the foods we introduced last summer? Are we damaging his esophagus without knowing? Should we have scoped after each food? What if the dairy allergy Carter outgrew that we believed never contributed to his EoE, was actually contributing to his EoE, but not as much as the soy… is that why he doesn’t have any symptoms? What if he does feel something when he eats, like tightness in his throat, but he just thinks it’s normal so he never says anything?
Why do I still not have a definitive answer about Winston? Does he have EoE, FPIES or regular IgE food allergies? Do I need a definitive answer if he is symptom free? Why was his scope clean in the middle of his vomiting spell – wouldn’t there have been at least one eosinophil in his biopsies if he did have EoE? Could he have a mild case of FPIES without the diarrhea? Could he have FPIES and an IgE allergy to oats simultaneously?
My initial thought was to call the gastroenterologist at Helen Devos Children’s Hospital who had scoped both of them to get her opinion, but as I recalled she didn’t seem too concerned about needing to re-scope either. Maybe there was something to that… maybe not. But I had reached my limit (again) and needed some answers. It was time to see a specialist.
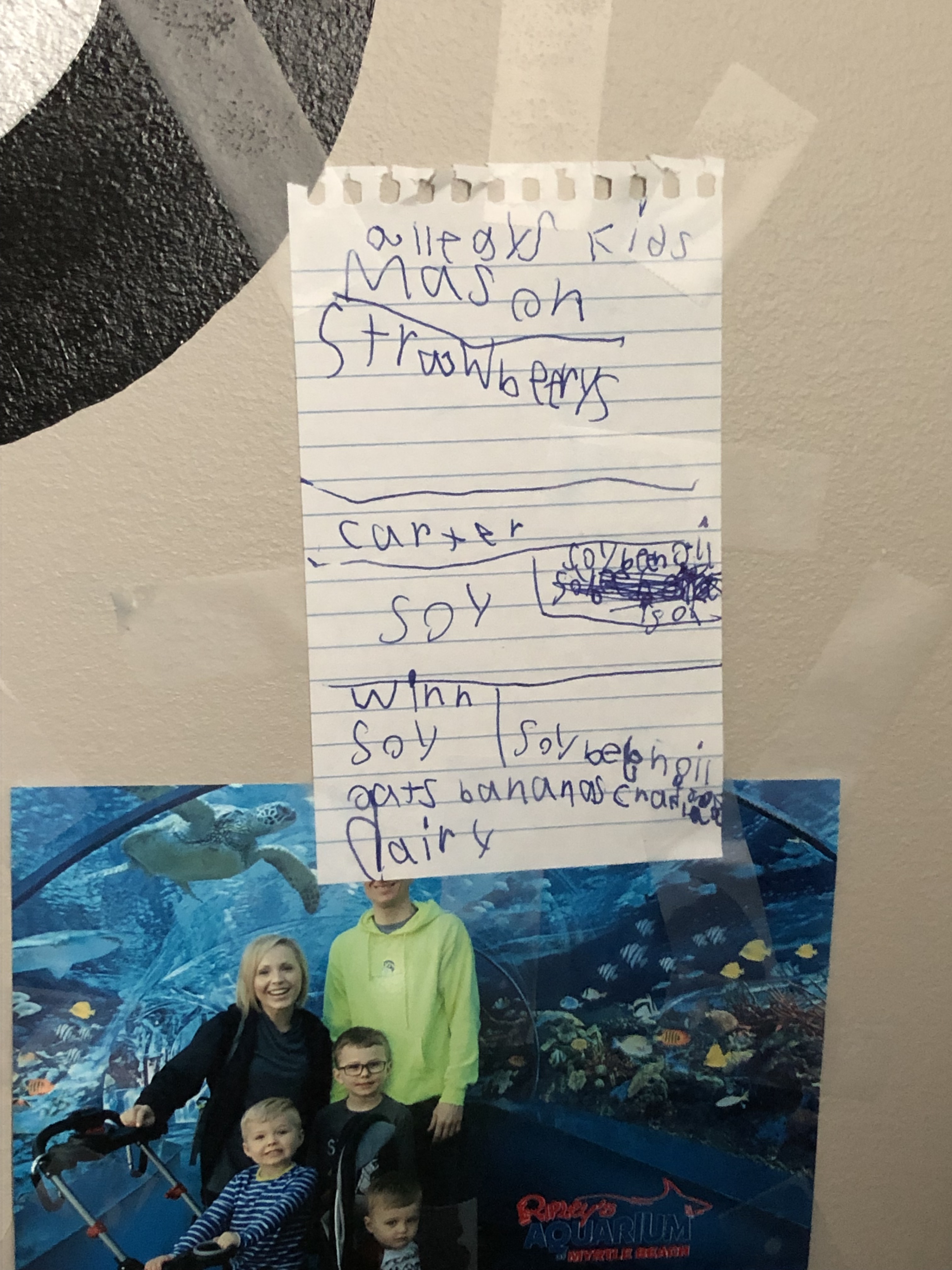
I called down to the University of Michigan Food Allergy Clinic in Ann Arbor and made appointments for all three of my boys. I figured since we were going down there anyway, might as well have Mason’s strawberry allergy re-evaluated too. Miraculously, they got us in on August 27th and 28th, the week before school started; Mason and Winston on the first day at one facility, Carter on the second day at a different facility.
If you know anything about University of Michigan medicine, you know they don’t let just anyone in; these physicians are at the top of their game and stay current on all medical practices. They are the best of the best. And of course, I did a little reading up on the physician we were seeing before our arrival. She was board certified in pediatrics and allergy/immunology, specializing in pediatric food allergies and asthma. She’s even doing EoE food allergy research with Johns Hopkins. We basically hit the allergist jackpot as far as I was concerned and I couldn’t wait to get answers to my questions.
Here’s what happened…
Mason – Strawberries
We started with Mason because he was the easiest. By that I mean his allergies have been the most “normal”, the easiest to diagnose. Mason has always had IgE-mediated food allergies, the kind that cause an immediate reaction upon ingestion of the food. He always broke out in hives, first from corn as an infant and then from strawberries at age 3. Our only question with his history was whether or not he did actually have a strawberry allergy, as he had broken out in hives a second time without eating any strawberries at all. So the allergist’s solution was simple.
“Let’s retest him for strawberries and see if it’s positive.”
She performed a skin prick test (SPT) on Mason’s arm. There were 4 pricks: one for strawberries, one for birch trees, one for a negative control and one for a positive control. The birch trees was solely used for size comparison, since Mason had tested highly positive to them in the past. And after 20 minutes of impatiently waiting (and a little crying because the welt from the birch was unbearably itchy), we were pleasantly surprised to see that strawberries was negative.

“You can go ahead and reintroduce strawberries to Mason. Start with a 1/4 of a strawberry on day 1. Wait 20 minutes. If nothing happens, give him another 1/4 of a strawberry. Then on day 2 give him a whole strawberry. If he has no reaction, it is safe for Mason to eat strawberries again.”
We were so excited! We couldn’t wait to get home and start testing!
Next up was little Winston. In preparation for our appointment, I gathered up anything that pertained to his health history. This included a 2-page summary of his symptoms and treatment, a copy of the puke log I created to track his vomiting, printed images of the endoscopy he had done last year and a photo album on my phone with pictures of his previous skin prick test results. I even had a picture of his vomit, you know just in case. Better to be over prepared than under!
We reviewed his health history summary in detail:
- Reflux-like symptoms from birth
- Projectile spitting up with the introduction of infant oatmeal, a connection we didn’t realize at the time
- Diet changes for mom (breastfeeding) without any relief
- Treatment with all of the reflux medications without any relief
- Positive allergy testing for soy
- Excessive vomiting with the introduction of Cheerios (26-31 times per day)
- Positive allergy testing for oats
- Endoscopy without visible EoE or reflux / negative for eosinophils in the biopsies
- Positive allergy testing for bananas and cocoa bean
- Treatment for EoE using Budesonide Slurry and food elimination
- Immediate vomiting after eating yogurt
- Gradual subsiding of vomiting over several weeks
- Reintroduction of dairy in June 2019 without any symptoms recurring
- Complete remission for a year
My biggest question for the doctor was whether or not we should re-scope Winston since we had recently introduced dairy back into his diet.
“Winston never had EoE. You cannot have Eosinophilic Esophagitis without the presence of eosinophils in the esophagus. I do understand this assumption from your allergist… EoE does run in families and it is more prevalent in boys. But Winston’s biopsies were negative. There is no reason to re-scope him. We won’t find anything.”
Smack forehead.
“If you are certain that the oats triggered the vomiting, I am slightly suspicious that he might have chronic FPIES, but it’s hard to say for certain. Usually chronic FPIES presents diarrhea and failure to thrive. Winston never had these symptoms. It’s also possible he may have an atypical IgE-mediated allergy to oats. He could have both. I think today we should retest him for oats, bananas and soy, but not the cocoa bean [because he’s had chocolate a couple times without any issues]. But this won’t tell us if he has FPIES. The only way to diagnose FPIES is to do an oral food challenge. Children commonly outgrow FPIES to oats by age 5, and since you know the oats made him very sick, I do not think we should reintroduce them until he’s older. There’s no reason to put him through that; oats are very easy to eliminate from the diet.”
Let me back up for a moment. Food Protein Induced Enterocolitis Syndrome (FPIES) is a rare allergy that affects the gastrointestinal tract. The Asthma and Allergy Foundation of America defines (FPIES) as “a non-IgE mediated immune reaction in the gastrointestinal system to one or more specific foods, commonly characterized by profuse vomiting and diarrhea… FPIES reactions almost always begin with delayed onset vomiting (usually two hours after ingestion, sometimes as late as eight hours after). Symptoms can range from mild (an increase in reflux and several days of runny stools) to life threatening (shock)”.
There are two forms of FPIES: Acute (immediate and severe) is when the allergen is eaten once and symptoms present 1-6 hours after ingestion. Chronic (constantly recurring) is when mild and intermittent symptoms present after frequent exposure to the allergen. The most common triggers for FPIES are first foods like dairy and soy. Other common triggers are grains like rice, barley and… oats.
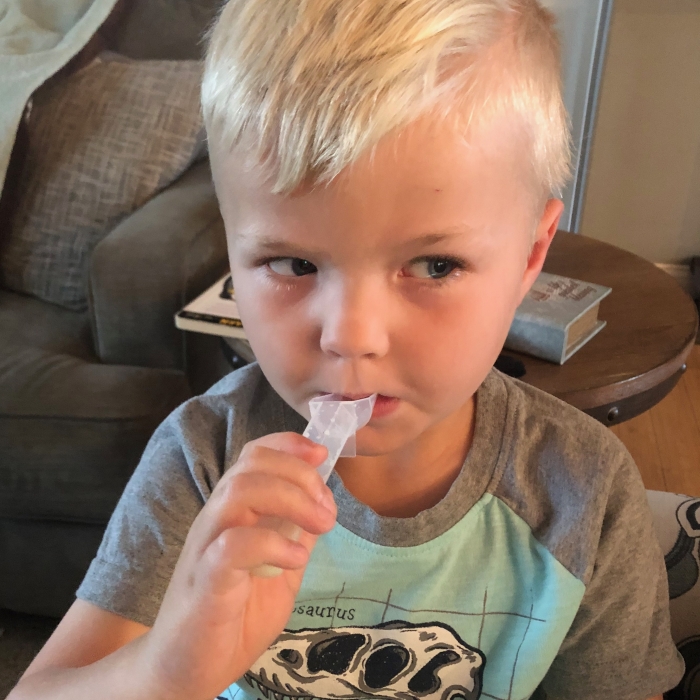
We retested Winn for soy, bananas and oats. You guys… they were all negative!


“You can reintroduce bananas and soy to Winston at home. Start with a small amount and gradually increase over 10 days. You are looking for delayed vomiting, usually 2-4 hours after eating. I will write you a prescription for Zofran in case he does have a reaction; this will stop the vomiting. Make sure he’s feeling better before you start.”
[Side note: poor little Winn started running a fever the day before we headed to Ann Arbor. The night at the hotel it was up over 102°. Fun times!]
So we agreed to wait on the oats oral food challenge until he was older but to move forward with other testing at home after he was over his little bug.
Day 2 in Ann Arbor and it was Carter’s turn. Though he has been in remission without medication for over a year, he’s the one who gave me the greatest concern. Similarly to Winston, I put together a complete health history for Carter with a list of my questions. I had a copy of my sleep log, just in case, along with photos of his previous SPT results and printed copies of his endoscopy. Together we reviewed Carter’s history:
- Reflux-like symptoms from birth
- Diet changes for mom (breastfeeding) without any relief
- Difficult feedings and increase in spitting up with the introduction of cow’s milk formula
- Treatment with all of the reflux medications without relief
- Symptoms resolving after beginning soy formula
- Gagging and vomiting on solid foods after 2 1/2 months of soy formula, a connection we did not make at the time
- Recurrent ear infections (7)
- Constipation
- Introduction of cow’s milk at a year causing diarrhea and irritability
- Pediatrician diagnosis of lactose intolerance – switch to soy milk
- Night wakings (2-4 times per night)
- Positive allergy test to dairy
- Night waking worsens (4-11 times per night) with excessive thirst (10-20 oz)
- Allergy test positive for soy
- Wean from Prilosec
- Allergy test mildly positive to tree nut, wheat, fish, sweet potato, vanilla, blueberry, coconut and sesame. Negative allergy test to dairy
- Endoscopy without visible EoE or reflux
- Biopsies with an eosinophil count of 6
- Allergist diagnosis of partially-treated EoE from removing all allergic foods
- Treatment with Budesonide Slurry and food elimination for over a year
- Patch test for food allergens in March 2018 with a positive result to soy
- Reintroduction of all food allergens (except soy) over several months without symptoms recurring
- Complete remission without medication for over a year
Although Carter had shown no symptoms after reintroducing all of his potential allergens, our concern was that symptoms aren’t always present with a relapse in EoE. Did we need to re-scope to be certain?
“Should he have been scoped after he was off of the Budesonide? Or after each food we reintroduced?”
“Probably. But it’s difficult to analyze whether or not Carter had EoE for certain in retrospect. His eosinophil count was only 6 and as you know it must be greater than 15 to diagnose active EoE. Could the elimination of foods have partially treated it? Possibly. He also may have been PPI [e.g. Prilosec] responsive; we now know that some people have relief from EoE by taking PPIs. If any of the foods you have already reintroduced were actually a trigger for him, I would have expected to see some symptoms after a year of ingestion. If it had only been 2 months, I would say lets scope. But we would have noticed something by now. I think we should retest for soy today to determine what we do moving forward.”
[Edit: In a follow-up email, I questioned the allergist’s opinion that Carter may not have ever had EoE, as his eosinophil count was only 6. She confirmed that there are only two reasons why one would have eosinophils present in the esophagus: EoE or a history of severe reflux. And as I reiterated that there was absolutely no evidence of any reflux in Carter’s scope (according to our GI’s analysis), she agreed that he must have had EoE that had been treated with food elimination and/or PPIs.]
So we performed another SPT on Carter to check for soy. The poor kid screamed before, during and after the entire thing. And he is LOUD. But we powered through with YouTube Kids videos and ice cream bribery!

And holy cow, it was negative! The first time in years!
“I want you to reintroduce soy into Carter’s diet when you get home using soy milk. Start with 1/4 tsp of soy milk on the first day, then gradually increase the amount for about a week or so. After that, he can have soy protein in all forms. We are looking for symptoms of abdominal pain, gagging, food impaction, vomiting, food aversion and night waking. If in the future he presents any of these symptoms, then an endoscopy would be needed.”
“What about soy lecithin? We were told that soy oil was safe but to avoid soy lecithin.”
“Soy lecithin is actually safer than soy oil. There is never any soy protein in soy lecithin. People who are anaphylactic to soy can usually eat soy lecithin.”
Smack forehead.
The doctor laughs. “You don’t need to worry. I do not see anything alarming about the way your primary allergist has treated your boys. Sometimes it’s difficult to diagnose these diseases and we have to make assumptions.”
On our drive home my head was in such a fog. My husband kept asking me why I wasn’t happier. I had been so worried we were taking a huge step backward but after our appointments it seemed we had made even more progress than before. Minus the possible FPIES diagnosis, it appeared that our kids might be on their way out of the food allergy phase; I knew for sure Winston did not have EoE and all of their skin tests were negative. So why was I not jumping for joy? I think the problem is my Type A personality just doesn’t favor the “unknown”. I struggle with not having definitive answers. But the past is the past and there’s no way to go back and make different decisions. Some things will remain unknown, and we just have to let them go, as long as we continue to move forward.
As I am reflecting on my feelings now, I ask myself… am I upset with our primary allergist for things he could have done differently? The short answer is no. Our allergist was our saving grace. So maybe we should have scoped Carter last year or maybe Winston didn’t need the Budesonide because he never had EoE; maybe Carter could have been eating a dozen more foods containing soy lecithin that we never allowed him to have. Does it really matter? No. Because in the grand scheme of things, our allergist made my children feel better; he took away their pain and discomfort. For that I will be eternally grateful.
And to the rude woman who turned my world upside down and made me question literally everything we had done over the past few years, if it wasn’t for your comment we probably wouldn’t have the answers we now have today. So for that I wholeheartedly thank you [heart emoji].
[See If At First You Don’t Succeed for the results of our at-home allergy testing. Don’t forget to subscribe!]